Wellness, Health Promotion, and Disease Prevention:
Wellness is a complex and multidimensional concept that involves optimizing health and promoting well-being. It encompasses the physical, mental, emotional, spiritual, social, and environmental aspects of a person. Wellness is more than just the absence of disease, it is the active pursuit of living life to its fullest potential. Health promotion and disease prevention are key components of achieving wellness. This essay will provide a comprehensive overview of wellness, health promotion, and disease prevention. It will examine the determinants of health, health promotion strategies, levels of prevention, and barriers to adopting healthy behaviors. In this article, we cover the key aspects of Wellness Health Promotion and Disease Prevention, providing practical strategies to improve overall well-being and prevent illness.
Read More: Mental Health Disorders Disturbed Everyday Activities
Determinants Wellness Health Promotion and Disease Prevention

There are a range of social, economic, and environmental factors that influence health outcomes. These factors are known as determinants of health. Some key determinants include income and social status, education, physical environment, employment and working conditions, social support networks, genetics, health services, gender, and culture. These determinants shape health behaviors and subsequent health outcomes. Low socioeconomic status is consistently linked to higher rates of disease, disability, and premature mortality across populations.
Those with lower levels of education also have poorer health indicators. The physical environment can facilitate or impede opportunities for physical activity, access to healthy foods, and transportation options. Employment conditions impact stress levels and the risk of workplace injuries. Strong social ties are associated with better health through social support. Genetics also play a role, but behavioral and environmental variables tend to have more influence on population health overall. Access to high-quality healthcare services is vital for health promotion and disease prevention. Gender norms and cultural values also affect health behaviors. Addressing these upstream health determinants through health promotion interventions can create the context for individuals to adopt healthier lifestyles.
Read More: wellness health promotion and disease prevention
Health Promotion Strategies

Health promotion involves enabling people to increase control over their health and supporting behaviors, environments, and policies that promote health and well-being. Various health promotion strategies can be implemented at the individual, community, and population levels. At the individual level, strategies focus on equipping people with knowledge and tools to make healthier choices and reduce risky behaviors. This can involve counseling, motivational interviewing, self-care education, and behavior change interventions. Community-level health promotion targets social norms and aims to build environments that support well-being.
Examples include worksite wellness programs, community walking groups, farmers markets, community gardens, and smoking restrictions in public places. At the societal level, health promotion policy aims to tackle the broader determinants of health and reduce health inequities. Policies can include tobacco taxation, active transportation infrastructure, healthcare system reforms, paid parental leave, and poverty reduction strategies. A comprehensive approach would utilize multiple health promotion strategies across these different levels.
Levels of Disease Prevention

Disease prevention efforts aim to reduce the onset and burden of acute and chronic health conditions. There are three main levels of preventive interventions: primary, secondary, and tertiary prevention. Primary prevention aims to stop the onset of disease. Vaccinations, smoking cessation programs, and blood pressure screening are examples of primary prevention. Secondary prevention involves detecting and addressing diseases in their earliest stages before symptoms emerge.
Screening programs for breast cancer, colon cancer, and cervical cancer allow early treatment that can prevent progression and complications. Tertiary prevention limits the effects of already established diseases through treatment and rehabilitation interventions. Managing diabetes with insulin therapy and lifestyle changes is an example. Primary prevention is the most cost-effective, avoids human suffering, and provides universal population benefits. However, balancing resources across all three levels of prevention is needed for an optimal health system.
Barriers to Health Behavior Change

While many health behaviors such as diet, exercise, and smoking are modifiable, changing habitual lifestyle patterns is extremely challenging. There are numerous barriers that individuals face in trying to adopt healthier behaviors. Intrapersonal barriers include lack of motivation, difficulty breaking habits, lack of time, fatigue, stress, and forgetfulness. Social and cultural norms can also discourage healthy behaviors. Environmental barriers like lack of access to affordable healthy foods or safe areas to exercise also play a role.
Health literacy issues, misinformation, and lack of actionable knowledge on how to make changes can also impede behavior change. Psychological issues like depression and anxiety interfere with motivation and self-efficacy. Other obstacles include physical limitations, family obligations, and inhibitive workplace environments. Financial barriers to preventive health services, nutrition education, gym memberships, and smoking cessation aids also impact health behaviors. Multi-component health promotion interventions that address these barriers on multiple socioecological levels have the greatest chance of facilitating positive behavior change.
Nutrition

Proper nutrition is vital for maintaining health and preventing chronic diseases. Achieving a balanced diet helps provide the body with optimal levels of macro and micronutrients. However, many Americans have poor diet quality falling short of recommendations for fruits, vegetables, whole grains, lean proteins, and fiber while exceeding limits for sodium, sugar, and unhealthy fats. This can lead to obesity, cardiovascular disease, type 2 diabetes, and certain cancers.
Improving nutrition requires a multi-tiered approach. At the individual level, nutrition education and counseling can empower people to make healthier food choices. Community-level efforts like increasing access to affordable produce through farmers’ markets and community gardens can make healthy eating more possible in underserved neighborhoods. At the societal level, policies such as the taxation of unhealthy foods, agriculture subsidies for fruits and vegetables, nutrition labels, and limits on marketing junk food to children are needed to promote healthy eating patterns. A culture of nutrition and well-being must also be fostered starting from a young age.
Physical Activity

Regular physical activity is one of the most important behaviors for preventing chronic diseases including heart disease, stroke, diabetes, and cancer. It helps control weight, strengthens bones and muscles, improves mental health, and increases longevity. The recommended minimum is 150 minutes per week of moderate activity or 75 minutes of vigorous activity in addition to muscle-strengthening exercises twice weekly. However, 80% of American adults do not meet these guidelines.
Barriers include lack of time, motivation, access to safe spaces for exercise, and sedentary lifestyles. Social support from family and friends has been shown to increase exercise adherence. Worksite wellness programs with active breaks, walking meetings, and gym access can promote activity during the day. Urban planning and policies that foster active transportation like walking and cycling infrastructure are beneficial. Mass media campaigns, apps, and wearable devices that track activity can also facilitate behavior change at the broader population level. Exercise recommendations should adapt to individual capacities and limitations rather than taking a one-size-fits-all approach.
Smoking Cessation

Tobacco use remains the leading preventable cause of morbidity and mortality worldwide. It increases risks for cancer, heart disease, and chronic obstructive pulmonary disease, stroke, and lung diseases. Quitting smoking significantly lowers these risks and improves health almost immediately. However, nicotine is highly addictive making smoking cessation very difficult.
A multifaceted approach combines counseling, social support, medication therapy, telephone quit lines, and media campaigns. Counseling helps develop problem-solving and coping skills for cravings and relapse prevention. Medications like nicotine replacement therapy, bupropion, and varenicline can help manage withdrawal symptoms. Text messaging interventions can provide tips and boost motivation. Mass media counter-marketing highlights the deceptive practices of the tobacco industry and smoking hazards. Tobacco taxes and smoke-free policies also motivate quit attempts. Many smokers require multiple quit attempts and ongoing follow-up and support.
Stress Management
Chronic stress can negatively impact nearly everybody system. It contributes to high blood pressure, heart disease, obesity, diabetes, anxiety, depression, headaches, gastrointestinal issues, and premature aging. Chronic stress results from factors like difficult relationships, financial strain, work pressures, and major adverse events. Effective stress management helps mitigate these effects.
Relaxation techniques including deep breathing exercises, meditation, yoga, and massage therapy can activate the body’s relaxation response and lower stress hormones. Physical activity can also alleviate tension. Assertiveness training helps establish boundaries. Reframing stressful situations, humor, optimism, and social support improve coping capacity. Supplements like ashwagandha, omega-3 fatty acids, and lemon balm may assist with stress adaptation. Stress management should adopt a whole-person perspective and target sources of stress across multiple domains of life.
Sleep Health

Adequate sleep is vital for cognition, mood, cardiovascular health, metabolism, immune function, and longevity. The recommended amount is 7-9 hours per night for adults. However, an estimated 30% of adults report insufficient sleep. Barriers to healthy sleep include work and social demands, stress, noise, light exposure from screens, and sleep disorders.
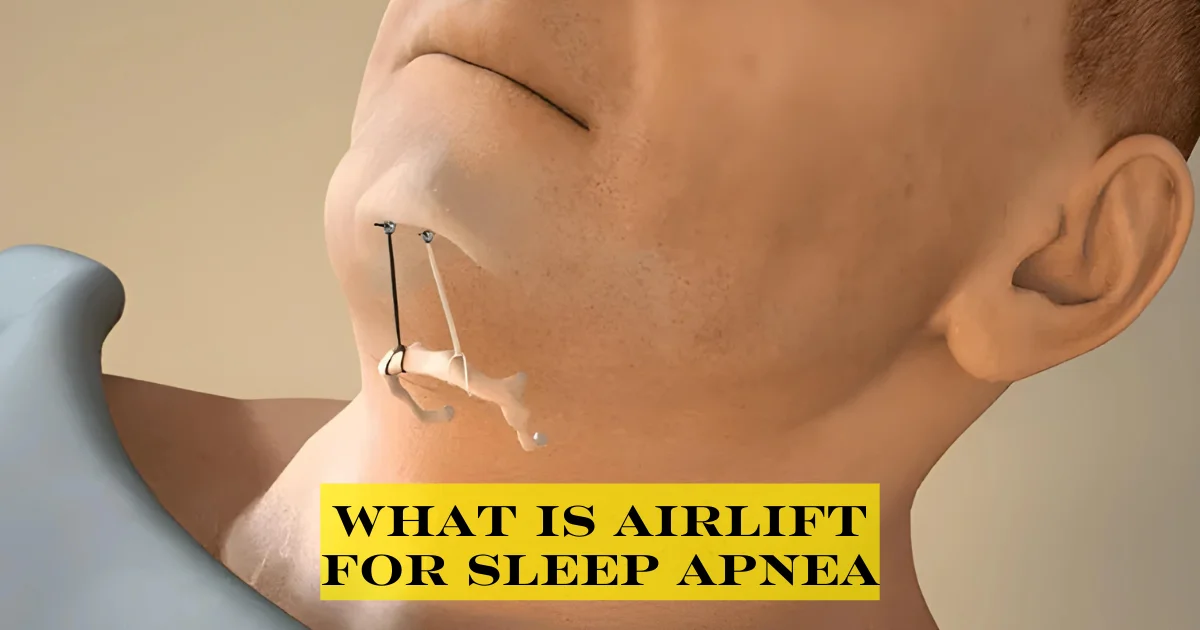
Behavioral sleep interventions aim to improve sleep hygiene through limiting daytime naps, establishing regular sleep schedules, darkening bedrooms, avoiding electronics before bed, and adopting soothing pre-bed rituals like reading. Exercise and avoiding caffeine in the evenings may also improve sleep quality. Relaxation techniques help lower stress hormones that interfere with sleep. Cognitive behavioral therapy addresses dysfunctional beliefs, anxiety, and maladaptive behaviors that contribute to chronic insomnia. Sleep apnea, restless leg syndrome, and other disorders may require further clinical treatment. Prioritizing sleep is essential for both physical and mental well-being.
Substance Abuse Prevention
The misuse of legal and illegal drugs exacts steep costs to individual and public health. Substance abuse contributes to violence, injuries, addictions, organ damage, cancers, and infectious disease transmission. Effective prevention requires comprehensive strategies across all levels of the social ecology. Community-based education campaigns can counteract misperceptions of social norms and harm, as most youth overestimate peer drug use. Media literacy programs also reduce the glorification of drugs and alcohol.
Policy options include increased taxation, limiting alcohol outlet density, raising the legal drinking age, and holding retailers accountable for underage sales. Screening by healthcare providers facilitates early intervention. School policies and drug testing aim for deterrence and linkage to counseling. However, zero-tolerance policies are less effective than approaches emphasizing social inclusion. Harm reduction like syringe access programs should also be supported. A strong foundation of family, school, and community that fosters healthy norms and connections is the most protective.
Mental Wellbeing

Mental health affects thinking, emotions, behaviors, relationships, and quality of life. Poor mental health contributes to lost work productivity, disabilities, addictions, and chronic disease risks. Positive mental well-being requires a supportive context to realize potential, cope with stresses, maintain relationships, and contribute meaningfully to the community. At the individual level, self-care practices like exercise, sleep, healthy eating, relaxation techniques, and mindfulness build resilience. Screening and treatment for depression, anxiety, and other conditions improve functioning. The social connection provides support. Worksites can promote work-life balance and stress management. Schools teach children emotional intelligence skills and social problem-solving. Governments and insurers must also expand access to mental healthcare. Holistic wellness requires integrating physical and mental well-being through relationships, purpose, and community.
Achieving wellness is not just an individual responsibility, but a societal one. Multifaceted strategies across intrapersonal, interpersonal, institutional, community and public policy realms are needed. Health education and literacy foster the skills and agency to make healthier choices. Social networks and social norms must promote well-being. Healthy environments where the default choice is the healthy choice facilitate lifestyle changes. Healthcare access is vital, but socioeconomic and educational policies may exert greater population health impacts. There is no single solution or quick fix. Sustainable change requires tackling upstream determinants across sectors. With concerted efforts, health promotion and disease prevention can build a culture and context where wellness is truly valued and attainable for all.