Introduction
Kidney disease and skin conditions often go hand-in-hand. Chronic kidney disease (CKD) can lead to a variety of skin problems, either as a direct result of the kidney dysfunction or as a side effect of kidney disease treatment. Conversely, many skin diseases have systemic effects that can impact kidney function.
Understanding the relationship between kidney disease and skin conditions is important for effective diagnosis and management of both types of disorders. This essay will provide an overview of common skin conditions associated with CKD, the effects of kidney dysfunction on the skin, skin problems related to kidney disease treatment, and kidney complications of primary dermatologic diseases.
How Kidney Disease Impacts Your Skin Condition—Revealed! Explore how kidney disease can silently alter your skin condition, from dryness to rashes. Uncover key connections for healthier skin with CKD. Chronic kidney disease (CKD) can lead to a variety of skin problems, either as a direct result of the kidney dysfunction or as a side effect of kidney disease treatment.
Read More: Mental Health Disorder Disrupt the Everyday Activities
Kidney disease encompasses various conditions that disrupt renal function, leading to impaired filtration and regulation. The two primary categories of kidney disease are acute kidney injury (AKI) and chronic kidney disease (CKD).
Acute Kidney Injury: AKI is characterized by a sudden decline in kidney function, often due to conditions such as dehydration, infections, medications, or severe illnesses. It can be reversible if diagnosed and managed promptly.
Chronic kidney Diseases: CKD is a progressive and irreversible deterioration of kidney function over time. It is typically categorized into stages based on the estimated glomerular filtration rate (eGFR), with stage 5 representing end-stage renal disease (ESRD) necessitating renal replacement therapy (dialysis or transplantation).
Skin Conditions Associated with CKD
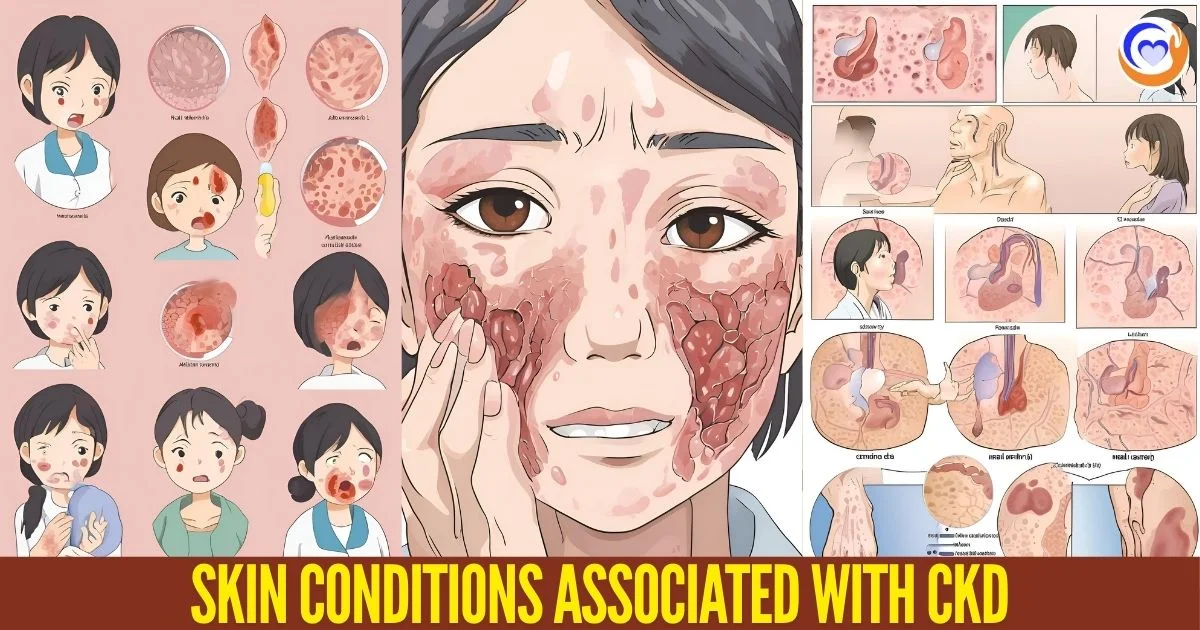
A number of skin disorders are more prevalent in patients with CKD. These include xerosis (abnormally dry skin), pruritus (itching), nail abnormalities, acquired perforating dermatosis, nephrogenic systemic fibrosis, uremic frost, and bullous dermatoses.
Xerosis: is the most common skin problem seen in CKD patients, occurring in up to 85% of patients on hemodialysis. The dry skin is related to fluid imbalances and electrolyte abnormalities caused by the kidney dysfunction. Pruritus, or itching, also affects a majority of advanced CKD patients, in up to 70-90% of patients on dialysis.
It can significantly reduce quality of life. The pathophysiology is not fully understood but likely involves systemic inflammation, accumulation of uremic toxins, secondary hyperparathyroidism, and dry skin.
Nail abnormalities: including half-and-half nails and Muehrcke’s lines are seen in up to 44% of CKD patients. Acquired perforating dermatosis is an uncommon condition featuring itchy papules with central crusting or ulceration. It tends to affect dialysis patients and can be associated with diabetes and nutritional deficiencies.
Nephrogenic systemic fibrosis: is a rare fibrosing skin condition that develops in CKD patients following gadolinium-based MRI contrast exposure. Thickening and hardening of the skin occurs, often preceding muscle and internal organ involvement. Uremic frost is a white powdery buildup of urea crystals that can develop on the skin of severely uremic patients, particularly in cold environments.
Bullous dermatoses: including bullous pemphigoid, porphyria cutanea tarda, and pseudoporphyria can also be associated with CKD. Binding of uremic toxins to keratin proteins in the skin may trigger these autoimmune blistering diseases in susceptible individuals.
Effects of Kidney Dysfunction on the Skin
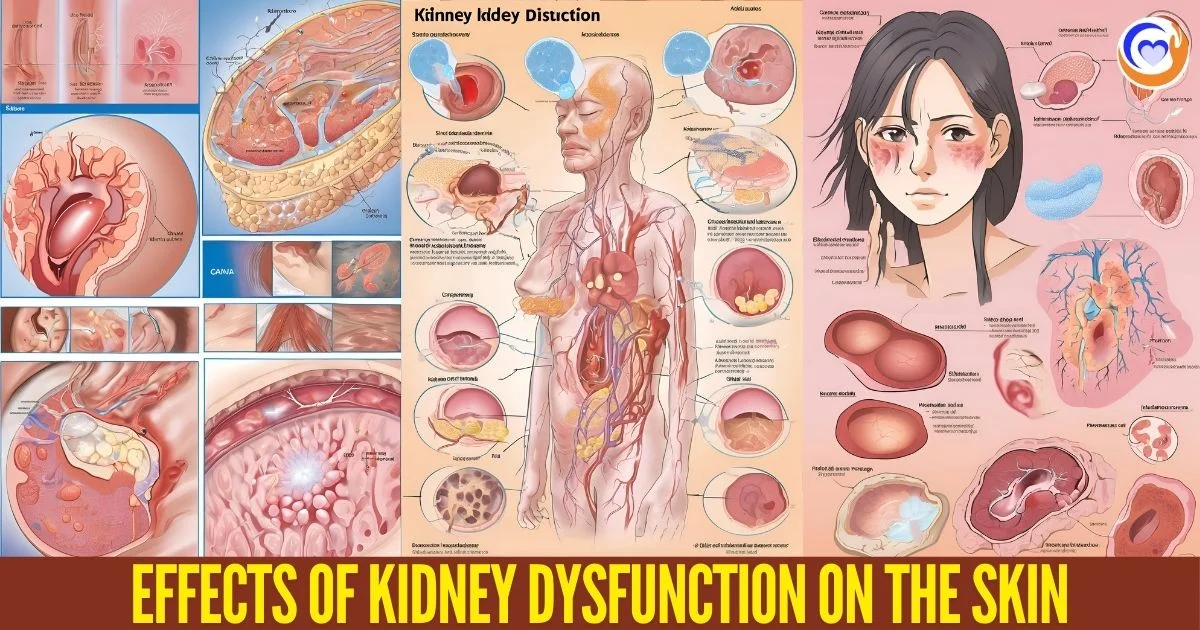
In addition to specific skin disorders, kidney disease has various direct effects on the structure and function of the skin. Fluid overload, electrolyte imbalances, and accumulation of uremic toxins play a role in many of the cutaneous issues of CKD.
Fluid overload and edema, commonly seen in kidney failure, can lead to skin swelling, stretching, and impairment of normal barrier functions. Electrolyte imbalances including hyperkalemia, hyperphosphatemia, and hypocalcemia alter skin homeostasis and integrity.
Buildup of uremic toxins also impacts the skin. Toxins like advanced glycation end products (AGEs) can cause collagen crosslinking and delayed wound healing. Elevated homocysteine may contribute to ulceration. Other toxins can trigger inflammation and pruritus.
Hormonal changes like secondary hyperparathyroidism also affect the skin, causing pruritus, calciphylaxis, and cutaneous neoplasms in advanced CKD. Anemia and nutritional deficiencies related to kidney dysfunction deprive the skin of oxygen and nutrients needed for self-repair.
Overall, the combination of fluid, electrolyte, nutrient, toxin, and hormone abnormalities in kidney failure alter the normal structure and physiology of the skin in ways that promote skin pathologies. Managing these systemic metabolic abnormalities can help improve cutaneous health.
Skin Problems Related to Kidney Disease Treatment
While kidney failure itself disrupts skin homeostasis, treatments for kidney disease can also trigger skin conditions. Management options like dialysis and kidney transplantation are lifesaving, but carry side effects that can impact the integumentary system.
Hemodialysis can be associated with a number of skin complications at the vascular access site. Infections are common, including bacterial infections and occasionally fungal infections. Other problems include ischemic ulcerations, aneurysms, and hemorrhages as vascular complications arise over time. Pruritus often worsens after starting hemodialysis, possibly related to dialyzer membranes or water impurities triggering inflammation.
Peritoneal dialysis also carries some skin-related effects. The dialysate fluid can irritate the peritoneal lining leading to infections like fungal peritonitis. Cutaneous complications include leakage of fluid through the peritoneal catheter exit site, causing local skin irritation. The catheter itself can erode through the skin if the external portion is not positioned properly.
Kidney transplantation improves kidney function and many CKD-related skin disorders. However, the immunosuppressive medications needed post-transplant pose their own dermatologic risks. Problems include increased skin cancer risk, particularly for squamous cell carcinoma and melanoma. Other possible side effects are more frequent viral infections like warts or herpes, and drug eruptions. Periodic skin cancer screening is recommended for all transplant patients.
While dialysis and transplantation treatments are critical for CKD patients, they must be managed carefully to minimize adverse effects on the skin. Ongoing dermatology care is an important component of treatment for kidney failure patients.
Kidney Complications of Skin Diseases
Just as CKD leads to secondary skin issues, certain primary dermatologic diseases have systemic effects on kidney function. Psoriasis, systemic lupus erythematosus, and other disorders can cause serious kidney complications.
Psoriasis: is an inflammatory skin condition that increases risk of CKD. The chronic inflammation and immune activity of psoriasis can promote kidney injury through cytokines, oxidative stress, and dysregulation of the renin-angiotensin system. Patients with severe psoriasis have up to a 2-fold increased risk of CKD. Periodic monitoring of kidney function is recommended in these patients.
Systemic lupus erythematosus (SLE): is an autoimmune disorder that commonly affects the skin and joints, but can also involve the kidneys. Lupus nephritis, kidney inflammation caused by SLE, occurs in up to 60% of SLE patients. Immune complex deposition in the kidneys triggers inflammation and scarring, leading to proteinuria, hematuria, and eventual kidney failure if untreated. Skin conditions like malar rash and photosensitivity aid in SLE diagnosis.
Certain inherited skin disorders have kidney complications as part of their systemic pathology. Epidermolysis bullosa, a blistering skin disease, can feature urinary tract involvement with repeated kidney and bladder infections. Fabry disease causes angiokeratoma skin lesions as glycolipid deposits accumulate in blood vessels, kidneys, and other organs. Managing the dermatologic manifestations and monitoring kidney function is important for these syndromic diseases.
The interplay between the skin and kidneys highlights the need for collaboration between dermatologists and nephrologists. Integrating care between specialties results in better patient outcomes. Ongoing research is elucidating the mechanisms behind many of the bidirectional relationships between kidney disease and skin disorders, which will inform future treatment innovations.
Read More: Kidney Disease Warning Signs
Conclusion
The skin and kidneys are intricately linked in homeostasis, so disruption of one organ often affects the other. CKD leads to increased incidence of many dermatologic issues either from the direct metabolic effects of kidney dysfunction or as side effects of dialysis/transplantation treatments. Conversely, certain primary skin diseases like psoriasis and SLE have secondary impacts on the kidneys.
Awareness of these associations facilitates prompt diagnosis and targeted management of both skin and kidney diseases in affected patients. A multidisciplinary approach with close dermatology-nephrology coordination is key to optimal patient care. Further research on the pathophysiologic pathways will open doors to better understanding and treatment of these related conditions in the future.
FAQs
Q: What types of skin conditions are associated with chronic kidney disease (CKD)?
A: Chronic kidney disease can lead to skin conditions like xerosis (dry skin), pruritus (itching), nail abnormalities, nephrogenic systemic fibrosis, uremic frost, and bullous dermatoses.
Q: Why does kidney disease affect skin health?
A: Kidney disease disrupts fluid and electrolyte balance, hormone levels, and toxin removal, leading to skin problems like itching, dryness, and infections.
Q: How does chronic kidney disease (CKD) lead to dry skin?
A: CKD can cause fluid imbalances and electrolyte issues, which result in dry skin (xerosis) in up to 85% of patients undergoing hemodialysis.
Q: What are the main effects of dialysis on skin condition?
A: Dialysis can lead to infections at the access site, skin irritation, pruritus, and in some cases, complications like ischemic ulcers and vascular access aneurysms.
Q: Can kidney disease treatments cause skin problems?
A: Yes, treatments like dialysis and kidney transplantation can cause skin issues, including infections, irritation, and increased cancer risks due to immunosuppressive drugs.
Q: How does kidney dysfunction contribute to pruritus (itching) in CKD patients?
A: Pruritus in CKD is likely caused by systemic inflammation, uremic toxins, and secondary hyperparathyroidism, affecting up to 90% of dialysis patients.
Q: What skin problems are commonly seen in patients on hemodialysis?
A: Patients on hemodialysis commonly experience dry skin, pruritus, nail abnormalities, and sometimes rare conditions like acquired perforating dermatosis.
Q: How do autoimmune skin diseases like lupus impact kidney health?
A: Autoimmune diseases such as lupus can cause lupus nephritis, where immune complexes deposit in the kidneys, leading to kidney inflammation and potential failure.
Q: What role do dermatologists play in managing CKD-related skin conditions?
A: Dermatologists collaborate with nephrologists to monitor and treat skin complications from CKD, helping to manage dryness, itching, and risks associated with dialysis and transplantation.
Q: Can skin diseases increase the risk of developing kidney problems?
A: Yes, diseases like psoriasis and lupus increase the risk of kidney complications due to chronic inflammation and immune response affecting renal function.