Let me tell What is prostatitis and how is it treated—it’s when your prostate gland gets all swollen and irritated, causing a real bother down there. The prostate is this little guy that sits right below your bladder and in front of your rectum, with the urethra—the tube that carries pee and semen out of your body—running smack through its center.
When it flares up, the tissue around it can get tender, and you might feel like everything’s off. I’ve seen buddies deal with this, and it’s no picnic—sometimes it’s from bacterial infections like UTIs (those pesky urinary tract infections), and other times there’s no clear cause. The good news? There are treatments to help manage those annoying symptoms, whether it’s meds or just tricks to ease the discomfort.
Read More: How a Gym Routine Can Help You Overcome Depression
What Are the Different Kinds of Prostatitis?
Now, prostatitis isn’t just one thing—it comes in four types, each with its own personality. There’s the acute kind, where bacteria hit fast and hard, bringing fever, chills, and painful urination that makes you wince; it’s suddenly there and needs antibiotics quick. Then you’ve got chronic bacterial prostatitis, a slower burn that doesn’t usually spike a fever but sticks around, making it tough to pee without pain or difficulty—it can take longer to treat.
The most common, called CPPS (chronic pelvic pain syndrome), hits about 1 out of 3 men, lingering for months or even years with pain in the pelvis, perineum (that area between your scrotum and rectum), and genitals—no infection here, just pure frustration. Lastly, nonbacterial prostatitis (or asymptomatic inflammatory prostatitis) is sneaky—it’s inflammation without symptoms, so you only learn you have it from tests for something else, and it doesn’t need treatment. From my chats with folks, these types can really mess with your day, but knowing what’s up helps you tackle it.
Prostatitis is a tricky thing—it’s when your prostate gland gets all worked up and inflammatory, causing a mess of issues. I’ve talked to guys who’ve been through it, and it’s no walk in the park. It can hit you suddenly with something acute or drag on gradually as a chronic condition, depending on what’s behind it. The good news is there’s treatment out there, like antibiotics for the bacterial kind or other ways to ease the pain and trouble. It’s all about figuring out what type you’ve got and tackling it head-on.
What Sparks Prostatitis and How Does It Feel?
Let’s flip the script—prostatitis isn’t always from bacteria, though that’s a big player. Sometimes it’s a sneaky infection that causes acute bacterial prostatitis, hitting you with fever, chills, and a painful time when you pee—it’s frequent, burns like hell, and doesn’t come easy, almost urinating with difficulty. Other times, it’s chronic bacterial prostatitis, where the pain and trouble still linger, but no fever usually comes along; it takes longer to treat.
Then there’s CPPS (pelvic syndrome), the most common, hitting approximately 1 out of 3 men—it’s a stubborn ache in your pelvis, perineum (that area between your scrotum and rectum), or genitals that can last months or years, and it’s not an infection. Lastly, nonbacterial or asymptomatic prostatitis is quiet—you may not experience symptoms, only learn you have it after tests for other stuff, and it doesn’t need medical help. I’ve seen how it varies—some buddies felt it unlike anything else, while others didn’t know until a doc said so.
Prostatitis can be a real pain—literally. It’s when your prostate gets all fired up with inflammation, and let me tell you, it’s no picnic. I’ve known folks who’ve dealt with this, and it’s all about finding the right way to calm it down. Whether it’s bacterial or something else, treatments vary—sometimes it’s meds to fight an infection, other times it’s just managing the symptoms like painful urination or pelvic discomfort. The key is to see a healthcare provider to figure out what’s up and how to tackle it.
Why Bacterial Prostatitis Happens and What It Feels Like
Let’s dive into the bacterial side of prostatitis—it’s a sneaky culprit that can cause a lot of trouble. Picture this: bacteria sneak in through your urethra or when urine flows backward, sparking an infection that hits hard with fever, chills, and aches—almost flu-like. I’ve heard buddies groan about the frequent urge to pee, only for it to stop and start with a sting (dysuria).
It’s different from nonbacterial types because it’s clear what’s to blame, sometimes from UTIs, catheter use, or even pelvic injury. The pain might spread to your lower back or abdomen, and if you’ve got stress or a wonky nerve, it can feel worse. For me, chatting with a doc was a game-changer—it’s important to note those changes and get help fast.
Prostatitis is a real hassle—it’s when your prostate gets inflamed and throws everything off. I’ve seen mates struggle with it, and it’s tough. It can happen from bacterial infections or other sneaky causes, and how it’s treated depends on what’s going on—sometimes it’s meds to fight bacteria, sometimes it’s just easing the pain. The trick is catching it early and figuring out if it’s the acute kind or something chronic that sticks around.
What Trouble Can Bacterial Prostatitis Stir Up?
Let’s talk about the mess bacterial prostatitis can kick up—it starts when bacteria get through your urethra or urine flows backward (vesicoureteral reflux), sparking an infection. I’ve heard of guys who ignored frequent UTIs or a recent bladder issue, and bam—it turned into something nasty like sepsis, a life-threatening condition that hits your whole body and needs immediate medical help.
Other headaches include sexual dysfunction or inflammation that spreads near your prostate, maybe from using a catheter, having a biopsy, or even pelvic injury. If you’ve got nerve damage, a history of this stuff, or you’re older than 50 with an enlarged prostate (benign prostatic hyperplasia), the risk increases—it’s all part of the potential factors that make it more likely.
Prostatitis is a real bother—it’s when your prostate gets all inflamed and throws you for a loop. I’ve seen it knock folks around with infection or just plain irritation, and figuring out how to fix it is key. Treatment might mean meds for the bacterial kind or ways to ease the discomfort if it’s something else. It’s all about spotting it and sorting it out quick.
What is prostatitis and how is it treated?
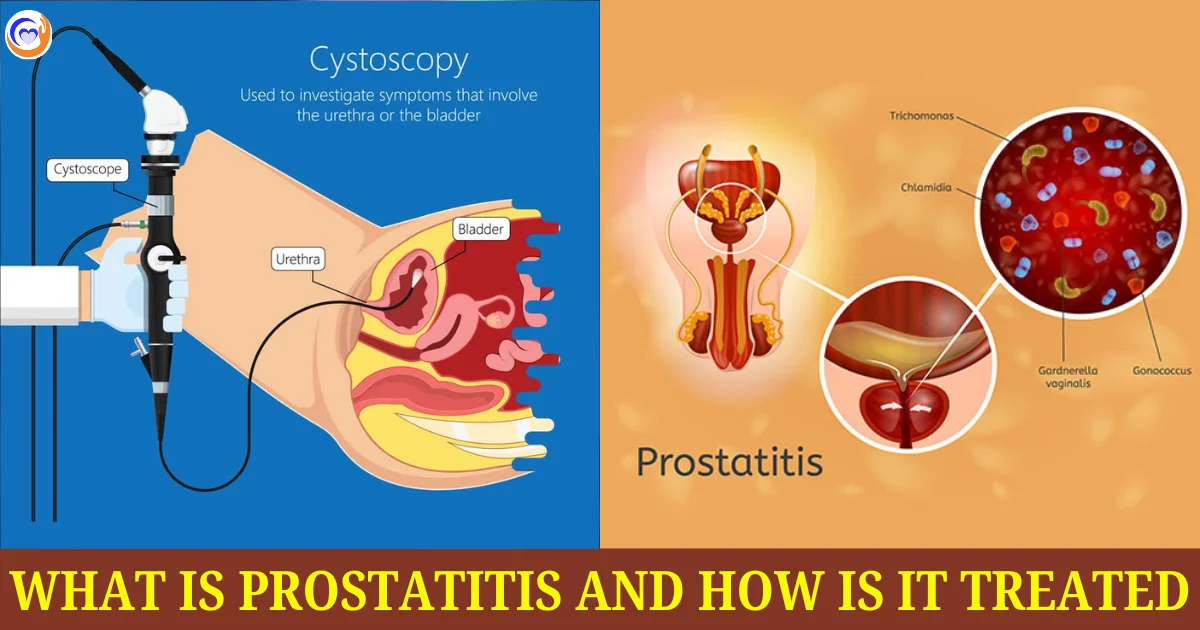
Let’s flip it—knowing what’s up with prostatitis starts with the doc digging in. They’ll assess how you’re feeling and poke around with a physical exam—think a digital rectal check where they insert a gloved, lubricated finger into your rectum (with your say-so) to check for pain or swelling. I’ve had buddies squirm through that, but it’s worth it—they might even massage the prostate to grab a sample of seminal fluid.
Then there’s urinalysis or a urine culture to spot bacteria, or a blood test for PSA (prostate-specific antigens) levels—high ones may hint at trouble like cancer, though prostatitis itself doesn’t increase that risk, staying benign and not cancerous. If it’s trickier, they’ll pull out bigger guns like cystoscopy—a pencil-sized lighted tube with a camera to peek inside your bladder and urethra—or a transrectal ultrasound to show abnormalities if antibiotics aren’t cutting it. It’s all to help determine what’s causing the fuss.
Conclusion:
Prostatitis is a beast, but it’s not unbeatable. Whether it’s a quick bacterial hit or a long-haul pain, knowing what you’re dealing with—symptoms, causes, fixes—makes it less of a boogeyman. Chatting with a doc’s the best move to wrestle it down and get back to normal.
Read More: Structure of Human Brain and Function
FAQs:
What Exactly Is Prostatitis?
It’s when your prostate—a little gland below your bladder and in front of your rectum—gets swollen and irritated. The urethra, that tube carrying pee and semen, runs right through it, so when it’s inflamed, things get messy. There are four types, and it can hit from bacteria or just pop up with no clear reason.
What Are the Types of Prostatitis?
There’s acute bacterial prostatitis—fast and nasty with bacteria causing it. Chronic bacterial prostatitis lingers longer, also from bacteria. Then you’ve got chronic pelvic pain syndrome (CPPS), the most common, sticking around with pelvis pain but no infection. Lastly, nonbacterial prostatitis is quiet—no symptoms, just inflammation found by chance.
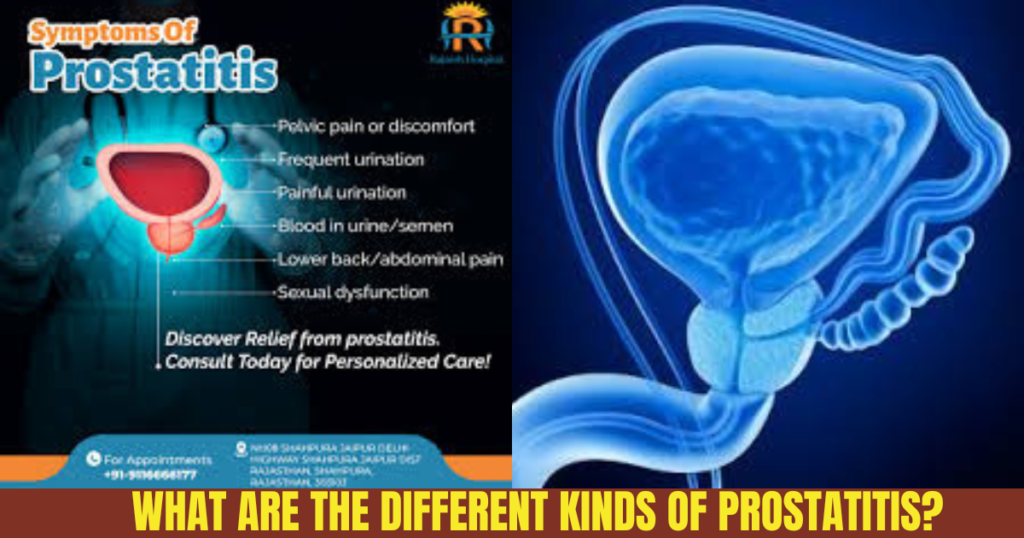
What Does Prostatitis Feel Like?
It varies. You might feel pain in your lower belly, genitals, or between your scrotum and rectum. Peeing can hurt or feel urgent, sometimes with blood in your pee or semen. I’ve heard guys say it’s like a constant ache, or worse during sex or ejaculation—sometimes even causing erection trouble.
What Causes Prostatitis?
Bacteria can sneak in through your urethra or backward urine flow, sparking bacterial types. For CPPS, it might be stress, nerve irritation, or muscle damage—no bacteria there. Sometimes, it’s a puzzle with no answer, which drives my mates nuts when they’re trying to figure it out.
Can Prostatitis Get Worse?
Oh yeah—if it’s bacterial, you could end up with sepsis, a scary body-wide infection needing a doctor ASAP. It might mess with your sex life or spread inflammation nearby. I’ve seen it throw curveballs, but it’s not cancer—that’s a relief, even if it mimics some signs.
How Do Doctors Spot Prostatitis?
They’ll ask about your symptoms and do a check-up. A finger in the rectum—yep, awkward—feels for swelling. Urine tests hunt bacteria, blood tests check PSA levels (high ones can confuse things with cancer), and sometimes they peek inside with a camera or ultrasound if it’s stubborn.
How Do You Treat Prostatitis?
If bacteria’s the culprit, antibiotics are your friend—quick for acute, longer for chronic. For CPPS or nonbacterial types, it’s about easing pain with meds, heat, or relaxation tricks. I’ve seen guys swear by warm baths to take the edge off when it’s acting up.
Who’s at Risk for This?
Guys with frequent UTIs, catheter use, or past prostatitis are prime targets for bacterial kinds. Older fellas over 50 with an enlarged prostate? Higher odds for all types. Nerve damage or pelvic injury ups the CPPS risk—life’s little hits add up.
Does Prostatitis Mean Prostate Cancer?
Nope—it’s benign, not cancerous, and doesn’t hike cancer risk. But here’s the kicker: it can raise PSA levels, just like cancer does, so extra tests might be needed to clear the air. That overlap spooked a friend of mine till the doc sorted it.
Can You Prevent Prostatitis?
It’s tricky—no surefire way, but keeping UTIs at bay helps the bacterial kind. Staying unstressed and avoiding pelvic knocks might dodge CPPS. I tell my pals to drink water and not hold their pee—simple stuff that might keep it from flaring.